WTF is Happening with the Perimenopause Bloating
CW: brief mention of intentional weight loss, special diet options (e.g., low-FODMAP), and lots of poop talk
While it's super common in perimenopause, bloating is an underserved topic.
I’m highly perimenopausal, sleepless, and night-sweating, and I’ve also had some significant bloating in the last couple of months. We need to be talking more about the bloat.
I’m out here looking for solutions, and across the interwebs, I find a bunch of consumer blogs offering generic advice that, in reality, are thinly veiled weight-loss ads. Bleh.
This riled me up and made me want a more weight-inclusive bloating solution, with more help and less harm.
Yes, bloating is not great for body image. Also, yes, we still need some better ideas for our tender, gassy tummies, not a calorie restriction plan.
Hi there, if we haven’t met yet, I’m Melinda Staehling. I’m an Oregon-based Certified Nutrition Specialist, Menopause Society Certified Practitioner, and today, your guide down the tube of digestion from mouth, to, well, toilet.
While niche, bloating is a favorite topic because when we get some relief, then wow, we’re all feeling better!
A few cautions before the meat and potatoes of the post:
⚠️ People with eating disorders have very high rates of co-occurring digestive concerns, which include bloating. If you have an active eating disorder or history, be extra gentle when implementing these steps, and please, work with your care team. Your eating disorder care comes first.
An example - I mention the low FODMAP diet as a possibility, below. That’s not a good option to undertake without your helping practitioners and a personalized, gentle approach.
⚠️ Bloating Red Flags
If your bloating is new and does not resolve with a bit of time and some of the methods below, it’s time to get in for some testing. Starting with your primary care Doc and following up with GI is a great idea.
⚠️ Supplements might help. There are a few points in the following article where I’ll mention supplements. None of these are affiliate links, and it’s a personal value of mine not to earn income from supplement sales.
⚠️ Last one! As y’all know, THIS IS FOR EDUCATIONAL PURPOSES ONLY. Always consult with your healthcare team before making changes to your plan. I’m a nutritionist, but I’m not your nutritionist, and I don’t diagnose or prescribe.
What is Perimenopausal Bloating?
Bloating is that uncomfortable feeling of trapped gas, abdominal pressure, and fullness.
Distension is the actual increase in abdominal size, which can feel like we’re blowing up like a balloon from the inside out. Sometimes, these two occur together, and they can also be separate symptoms (and need different solutions to find relief).
Bloating is complex and can have many different origins. It can occur alongside other GI issues. It’s highly correlated with IBS-C (constipation type) and other GI conditions like celiac disease and SIBO.
Here are some of the causes of bloating. For many of us, these can overlap:
Food intolerances: Sensitivities to certain foods such as lactose, gluten, or high-FODMAP ingredients may cause gas, abdominal pressure, and bloating. These reactions often occur when the body struggles to properly digest or absorb specific components of foods (like carbs or proteins).
Medications: Many prescription and over-the-counter drugs can cause bloating by slowing digestion, altering gut bacteria, or changing fluid balance. Hormonal medications, including the progesterone component in hormone therapy, can sometimes cause bloating.
Pelvic floor concerns: The pelvic floor muscles play a key role in supporting the intestines and aiding in bowel movements. When these muscles are either tense or weakened after childbirth, surgery, or chronic constipation, it can lead to trapped gas, pressure, and bloating.
Altered gut microbiome/gut dysbiosis: A shift in the balance of gut bacteria, for example, after food poisoning or antibiotic use, can cause fermentation along the gut path, leading to gas and bloating.
Sensory differences: People with neurodivergent traits (like autism or ADHD) often have heightened or altered sensory awareness. Sensory processing differences can also influence how certain textures or sensations in the gut are experienced.
SIBO: SIBO occurs when bacteria that normally live in the large intestine migrate into the small intestine. These bacteria ferment carbohydrates earlier in digestion, producing excess gas and bloating, often accompanied by abdominal pain, diarrhea, or constipation.
The methods to relieve bloating are as diverse as the causes themselves. Any combination of food, supplements, lifestyle, and medications might help you feel better.
While beyond the walls of our post today, techniques like biofeedback and gut-directed hypnotherapy show promising results for bloating relief.
What’s Up with Perimenopause and Bloating
In a study of 600 peri- and menopausal aged participants from age 44-73, a whopping 94% reported digestive health concerns, with bloating the top-reported symptom (74%) followed by constipation (54%).
So yes, compared to when we were in our 20s and could eat anything without fear of repercussion, the bloating is increasing.
It’s easy to turn to the hormonal aspect of perimenopause as a possible cause, but we need to be careful about that. Sure, the closer together and the increased number of perimenopause cycles could have something to do with it. I know PMS bloating is a thing for many of us.
We can also look at menopausal hormone therapy (MHT) as a possible cause of bloating. Taking progesterone (most commonly known as Prometrium) can cause bloating, especially during the hormonal waves of peri. While taking progesterone is recommended alongside the estrogen part of hormone therapy to protect the uterus from excess growth, it can come along with a range of side effects, bloating being one of them.
So we have increased menstrual cycles, taking progesterone as a medication, and a general increase in digestive concerns from aging as the (unwelcome) cherry on top.
A Word About Body Image in Perimenopause
Bloating can be annoying, and it might be pretty painful. It can also encourage body image distress and lead to an increase in disordered eating, eating disorder thoughts, and behaviors. What to do?
I know that around perimenopause, emotions can feel more tender (hello crying jag at my umpteenth Schitt’s Creek watch), so I think it’s important to consider how bloating affects our mental health, and do some checking in...
First, let’s boldly set realistic expectations about our bodies. While the media may portray washboard abs and a thin ideal, we know that’s not how bodies look. Stomachs are meant to expand as we eat, and gas tends to build up throughout the day. Those little gut bugs (aka your microbiome) are doing their jobs!
We also have shifting bodies in peri and beyond, with more weight concentrated in our mid-section. This can feel new and different, and lead to more negative body image.
READ MORE: A Weight-Inclusive Approach to Perimenopause Nutrition
So, here, I’m going to softly ask you to make some distinctions between the type of bloating and distention that we’re talking about.
There’s a range of bloating that is totally expected, like from increased fiber intake, eating throughout the day, and hormonal cycles. Some of this can be alleviated by a few of the suggestions below.
And, some of this is a part of being in a human body. Let’s temper our expectations around what is realistic for reducing our bloating with compassion for the bodies we live in.
First Step: Check in on Constipation
I’m listing out my decision tree of what I might go through with a client, so we’ll start with constipation.
Are you constipated? Read on.
Nope? Skip ahead.
Constipation is a biggie for bloat. Poop talk incoming.
Constipation increases with age, and so does the severity of the surrounding symptoms.
If you’re backed up, this is already uncomfortable. Then, there’s going to be some trapped gas behind the stuck stool, and that can lead to even more bloat. Oof.
In an analysis of the Seattle Midlife Women’s Health Study, the role of hormones was not found to be the cause of perimenopause constipation [1]. Still, the symptoms were more severe in the perimenopause timeline. The increase in constipation was more a result of stressors, tension, anxiety, and elevated cortisol levels.
Some things you can try for constipation:
Drinking Water
Sorry to start with the obvious, but are you hydrated? Everyone is unique, so you can check in with a urine color chart and add hydration from there.
Adding Fiber, Especially Soluble Fiber
Fiber, especially soluble fiber, pulls water into the colon and forms easy-to-pass stools. Some excellent sources of soluble fiber are beans, apples, seeds, whole grains, and artichokes. Think of the slipperiness of mixing flaxseed with water, or of chia seeds swelling when hydrated. That’s soluble fiber.
Please, be chill about this. Do not go from 0 to 60 overnight. For most people, we’re looking at 25-35 grams of total fiber per day. Here are some more examples of soluble fiber sources.
Adding in Supplemental Fiber like Psyllium
This is a type of soluble fiber, but it gets its own shout-out because it is the G.O.A.T.
You have the option of getting ground psyllium powder at the health food store, or the super-fine and Orange Tang flavored brand Metamucil. Or, the Kirkland knock-off, for my Costco peeps.
As with any fiber, we want to start low and slow, and increase tolerance. Some people get a little more gassy as they’re ramping up.
Be wary, there’s some diet-y language on the Metamucil bottles. This stuff is so great, Meta, can’t we let it stand on its own?
Making Time for the Toilet
Many of us can train ourselves to have a bowel movement at a predictable time of the day, most of the time. To do this, you do have to take some time out of your busy morning schedule.
Here’s the plan.
Allow yourself some time for the toilet. Drink your water and possibly coffee, eat some fiber as a prep, and get yourself a Squatty Potty. Sit, relax, and see if the magic is happening. You don’t need to take all day, but after a meal, take advantage of your GI tract's increased motility. If you’re lingering on the can for more than 5 minutes, it's time to get up and try a few other tactics.
Kiwis
Studies show that two kiwis per day can alleviate constipation. You get bonus points here for eating the skins.
Lifestyle Changes for Perimenopausal Bloating
Now that we’ve covered constipation, we’re going to go big picture.
Some of the following lifestyle suggestions are approachable enough, but I realize others are a lot to tackle (hello, improve your sleep, so simple, such ease), and they’re not going to change magically overnight.
Start with slow, attainable goals, and break the bigger ideas down into small steps:
Chewing your food more thoroughly
Wearing clothes that fit. Ditch the tight, too-small jeans.
Cutting back on gum chewing. Both the ingredients in the gum (like xylitol or sugar alcohols) and the increased air swallowing can contribute to bloat.
Getting some daily movement. A short walk after your meals can do wonders.
Getting adequate, restful sleep.
Limiting or quitting smoking and alcohol. I’m OK with being the killjoy here.
Other Supplements to Help with Perimenopausal Bloating
Here are a few more options that can help provide more immediate relief.
💊 Probiotics
Yes, there are some options here, but wow, this is where I see so many people (clients and providers alike) make costly mistakes. Cha-ching!
If you read the following carefully, you will know more about probiotics than 99% of the population.
Repeat after me - “I will never again pick a random probiotic off the shelf.”
Repeat again, “I will never buy a generic 'proprietary blend’ probiotic.”
The possible benefits of taking a probiotic supplement are strain-specific. That means, we match the specific strain, like Bifidobacterium longum 35624, with the particular complaint, like bloating.
We do not, under any circumstances, select something random or because we heard about it in an ad. As in life, if you’re picking the wrong product for the wrong job, you can end up doing more harm than good. (And quite possibly wasting your hard-earned dollars.
I recommend trying Align Probiotic (Bifidobacterium longum 35624), which has been supported by research for IBS-C and bloating. Take this probiotic once daily, with or without food.
🌿 Peppermint Oil Capsules (Not Tea)
Another research-backed option is peppermint oil capsules. There are many brands, and I recommend IBGuard because it's available at many grocery stores.
The capsules are a lot more concentrated than peppermint tea. So while peppermint tea sure is tasty and the hot drink may also be soothing, you’re not going to get the same results as a more concentrated capsule.
Beware the peppermint burps.
Some Foods to Consider for Perimenopausal Bloating
You might think it’s strange to put food choices at the bottom of the list, but I always want to keep as many foods in our plan as possible.
The lowest-hanging fruit here might be to check your labels. Some ingredients are known to contribute to bloat:
Beans are a clear choice, which you already know. With beans, I find that if people back off their beans for a bit and then reintroduce them really low and slow, like, a few tablespoons at a time, they’re able to tolerate the fiber much better. You can always try some Bean-O.
Sugar alcohols - These are ingredients like sorbitol, xylitol, and mannitol (erythritol usually not as much), and are sweeteners found in chewing gum and other lower-sugar products such as low-sugar cookies or sugar-free hot chocolate.
Indigestible fibers - commonly found in keto products or gluten-free breads containing methylcellulose. While this ingredient is found in some commercial brand laxatives like Citrucel, if you’re getting it in your food without realizing it, you may be contributing to bloat.
Here are a few more food options to think about:
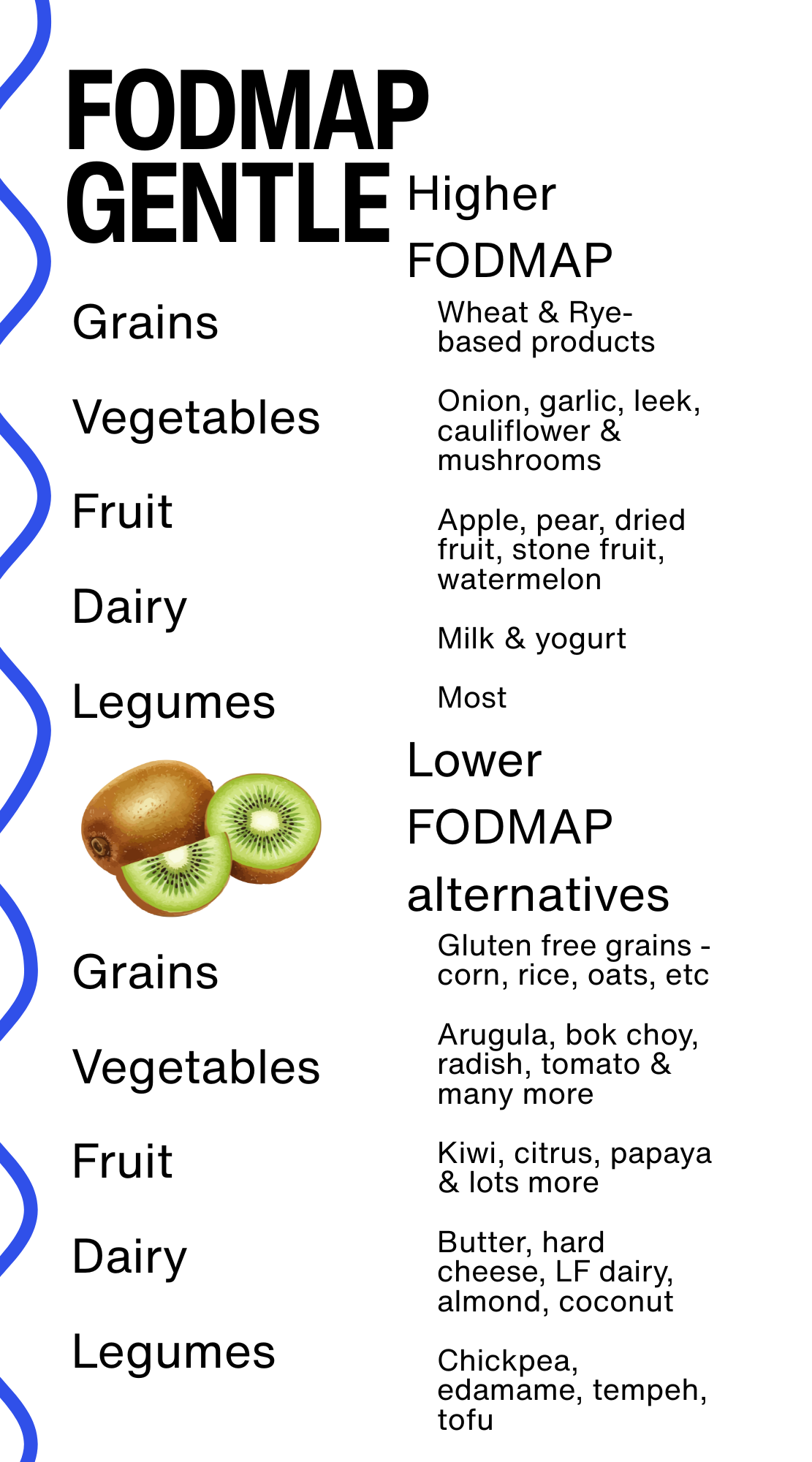
Low-FODMAP “Gentle”
You may have heard of FODMAPs before. What are they, exactly? FODMAPs are a group of carbohydrates that might possibly make your digestion feel worse. Why? They tend to ferment in the gut rapidly, which means that gas is building up. While some of us don’t notice much when we eat these foods, others get considerable symptoms, with bloating at the top of the list.
Here are some of the most common higher-FODMAP foods, along with an explanation of this process.
The real deal low-FODMAP plan can be a helpful plan to manage IBS. I believe it should be undertaken with the help of a trained professional. While it can be effective for IBS, it’s not a diet plan meant to be long-term, as it’s highly restrictive and lacking in fiber.
Even with the gentle approach described here, my vote is to bring in a professional if you want to go this route. I can help with this.
Try Lactose Free
It’s very common to be lactose intolerant. Depending on what population we’re looking at, up to 70% of people don’t digest lactose well, and so they don’t feel great after a bowl of ice cream.
Do a lactose-free trial to see if bloating improves, then add back a good amount of your favorite dairy as a test. If you have symptoms, playing around with Lactaid (or the generic) can help. Most people have a threshold of dairy that they can tolerate (i.e., you don’t have to give up dairy 100%), and there are a lot more lactose-free products available.
Wrapping it Up
This concludes our Tour de Perimenopause Bloating! I hope you found some new ideas to try for relief.
💙 Consider constipation.
💙 Build supportive lifestyle routines.
💙 Go easy with the supplements, but some might help.
💙 Check in with food from a gentle place.
💙 Honor where your body is at.
As a Certified Nutrition Specialist and Menopause Society Certified Practitioner, I’m here to help you navigate perimenopausal bloating and nutrition, while looking out for your relationship with food and your body. If you’re feeling overwhelmed by it all and would like a helping hand to guide you through some options, let’s chat. Please reach out here to book a free Introductory call.
I’m in network with many commercial insurance plans - check out this page for more info.